
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Cardiovascular Risk/Epidemiology
- Intensified Multifactorial Intervention in Patients with Type 2 Diabetes Mellitus
- Takayoshi Sasako, Toshimasa Yamauchi, Kohjiro Ueki
- Diabetes Metab J. 2023;47(2):185-197. Published online January 12, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0325
- 5,097 View
- 358 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
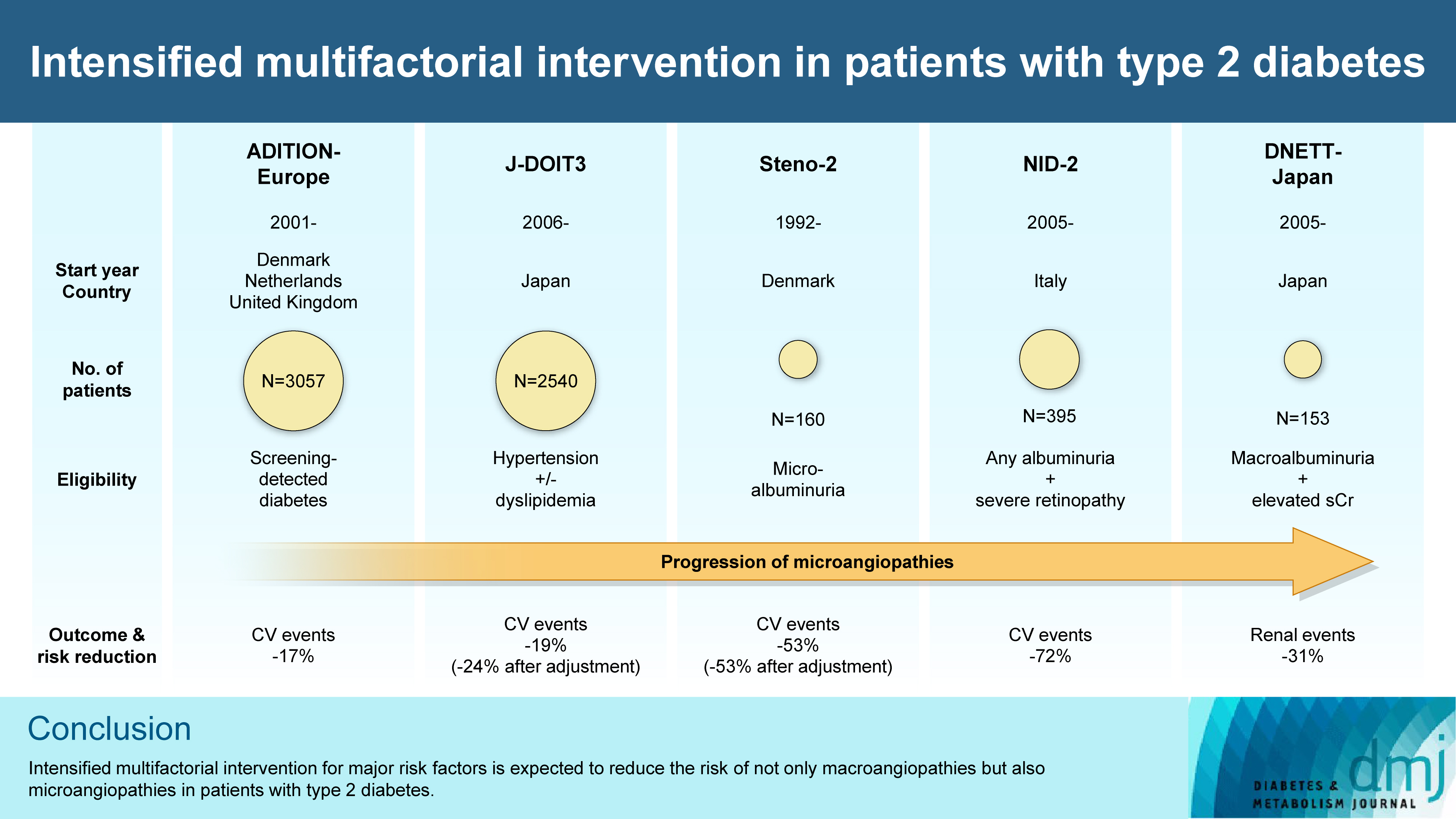
ePub - In the management of diabetes mellitus, one of the most important goals is to prevent its micro- and macrovascular complications, and to that end, multifactorial intervention is widely recommended. Intensified multifactorial intervention with pharmacotherapy for associated risk factors, alongside lifestyle modification, was first shown to be efficacious in patients with microalbuminuria (Steno-2 study), then in those with less advanced microvascular complications (the Anglo-Danish-Dutch Study of Intensive Treatment In People with Screen Detected Diabetes in Primary Care [ADDITION]-Europe and the Japan Diabetes Optimal Treatment study for 3 major risk factors of cardiovascular diseases [J-DOIT3]), and in those with advanced microvascular complications (the Nephropathy In Diabetes-Type 2 [NID-2] study and Diabetic Nephropathy Remission and Regression Team Trial in Japan [DNETT-Japan]). Thus far, multifactorial intervention led to a reduction in cardiovascular and renal events, albeit not necessarily significant. It should be noted that not only baseline characteristics but also the control status of the risk factors and event rates during intervention among the patients widely varied from one trial to the next. Further evidence is needed for the efficacy of multifactorial intervention in a longer duration and in younger or elderly patients. Moreover, now that new classes of antidiabetic drugs are available, it should be addressed whether strict and safe glycemic control, alongside control of other risk factors, could lead to further risk reductions in micro- and macrovascular complications, thereby decreasing all-cause mortality in patients with type 2 diabetes mellitus.
-
Citations
Citations to this article as recorded by- Exploring mechanisms underlying diabetes comorbidities and strategies to prevent vascular complications
Takayoshi Sasako
Diabetology International.2024; 15(1): 34. CrossRef - Targeting ERS-mitophagy in hippocampal neurons to explore the improvement of memory by tea polyphenols in aged type 2 diabetic rats
Wenjuan Feng, Chenhui Lv, Le Cheng, Xin Song, Xuemin Li, Haoran Xie, Shuangzhi Chen, Xi Wang, Lushan Xue, Cheng Zhang, Jie Kou, Lili Wang, Haifeng Zhao
Free Radical Biology and Medicine.2024; 213: 293. CrossRef - Risk of Dementia Among Patients With Diabetes in a Multidisciplinary, Primary Care Management Program
Kailu Wang, Shi Zhao, Eric Kam-Pui Lee, Susan Zi-May Yau, Yushan Wu, Chi-Tim Hung, Eng-Kiong Yeoh
JAMA Network Open.2024; 7(2): e2355733. CrossRef - Causes of In-Hospital Death and Pharmaceutical Associations with Age of Death during a 10-Year Period (2011–2020) in Individuals with and without Diabetes at a Japanese Community General Hospital
Minae Hosoki, Taiki Hori, Yousuke Kaneko, Kensuke Mori, Saya Yasui, Seijiro Tsuji, Hiroki Yamagami, Saki Kawata, Tomoyo Hara, Shiho Masuda, Yukari Mitsui, Kiyoe Kurahashi, Takeshi Harada, Shingen Nakamura, Toshiki Otoda, Tomoyuki Yuasa, Akio Kuroda, Itsur
Journal of Clinical Medicine.2024; 13(5): 1283. CrossRef - External validation of a minimal-resource model to predict reduced estimated glomerular filtration rate in people with type 2 diabetes without diagnosis of chronic kidney disease in Mexico: a comparison between country-level and regional performance
Camilla Sammut-Powell, Rose Sisk, Ruben Silva-Tinoco, Gustavo de la Pena, Paloma Almeda-Valdes, Sonia Citlali Juarez Comboni, Susana Goncalves, Rory Cameron
Frontiers in Endocrinology.2024;[Epub] CrossRef - Gut Microbiota Targeted Approach by Natural Products in Diabetes Management: An Overview
Priyanka Sati, Praveen Dhyani, Eshita Sharma, Dharam Chand Attri, Arvind Jantwal, Rajni Devi, Daniela Calina, Javad Sharifi-Rad
Current Nutrition Reports.2024;[Epub] CrossRef - Cardiovascular Risk Reduction in Type 2 Diabetes: Further Insights into the Power of Weight Loss and Exercise
Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(3): 302. CrossRef - Sarcopenia: Loss of mighty armor against frailty and aging
Takayoshi Sasako, Kohjiro Ueki
Journal of Diabetes Investigation.2023; 14(10): 1145. CrossRef
- Exploring mechanisms underlying diabetes comorbidities and strategies to prevent vascular complications
- Obesity and Metabolic Syndrome
- Perspective of Small-Molecule AdipoR Agonist for Type 2 Diabetes and Short Life in Obesity
- Miki Okada-Iwabu, Masato Iwabu, Kohjiro Ueki, Toshimasa Yamauchi, Takashi Kadowaki
- Diabetes Metab J. 2015;39(5):363-372. Published online October 22, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.5.363
- 6,789 View
- 61 Download
- 39 Web of Science
- 43 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Obesity associated with unhealthy diet and lack of exercise is shown to contribute to the onset and/or aggravation of the metabolic syndrome and diabetes, thus placing affected individuals at increased risk of cardiovascular disease and cancer. Plasma adiponectin levels are decreased in obesity, which causes insulin resistance and diabetes. Therefore, we identified adiponectin receptors (AdipoRs) as the therapeutic target. It was suggested that, similarly to caloric restriction and exercise, activation of the AdipoRs may have the potential not only to improve lifestyle-related diseases but to contribute to prolonged the shortened lifespan on a high caloric unhealthy diet. To this end, we have identified "AdipoRon" as an adiponectin receptor agonist. Indeed, AdipoRon ameliorated diabetes associated with obesity as well as to increase exercise endurance, thus prolonging shortened lifespan of obese mice fed on a high fat diet. Additionally, we have recently determined the crystal structures of the human AdipoRs. The seven-transmembrane helices of AdipoRs are structurally distinct from those of G-protein coupled receptors. It is expected that these findings will contribute not only to the elucidation of the AdipoR-related signal transduction but to the development and optimization of AdipoR-targeted therapeutics for obesity-related diseases such as diabetes.
-
Citations
Citations to this article as recorded by- Identification of a novel adiponectin receptor and opioid receptor dual acting agonist as a potential treatment for diabetic neuropathy
Oscar Ka-Fai Ma, Simone Ronsisvalle, Livia Basile, Ariya Weiman Xiang, Cristina Tomasella, Federica Sipala, Matteo Pappalardo, Koon-Ho Chan, Danilo Milardi, Roy Chun-Laam Ng, Salvatore Guccione
Biomedicine & Pharmacotherapy.2023; 158: 114141. CrossRef - AdipoRon Effect on Expression of Lipid Metabolism Genes in Cultured Human Primary Macrophages
I. A. Pobozheva, K. V. Dracheva, S. N. Pchelina, V. V. Miroshnikova
Molecular Biology.2023; 57(4): 616. CrossRef - The Antiviral Potential of AdipoRon, an Adiponectin Receptor Agonist, Reveals the Ability of Zika Virus to Deregulate Adiponectin Receptor Expression
Daed El Safadi, Grégorie Lebeau, Jonathan Turpin, Christian Lefebvre d’Hellencourt, Nicolas Diotel, Wildriss Viranaicken, Pascale Krejbich-Trotot
Viruses.2023; 16(1): 24. CrossRef - The Effect of Adiporon on Lipid Metabolism Genes Expression in Human Macrophages
I. A. Pobozheva, K. V. Dracheva, S. N. Pchelina, V. V. Miroshnikova
Молекулярная биология.2023; 57(4): 623. CrossRef - The effects of high intensity-interval training on vaspin, adiponectin and leptin levels in women with polycystic ovary syndrome
H. Ş. Aktaş, Y. E. Uzun, O. Kutlu, H. H. Pençe, F. Özçelik, E. Ö. Çil, L. Irak, Ö. Altun, M. Özcan, N. Özsoy, Ş. Aydın Yoldemir, S. Kalyon, Y. Arman, T. Tükek
Archives of Physiology and Biochemistry.2022; 128(1): 37. CrossRef - G protein-coupled receptors that influence lifespan of human and animal models
Francisco Alejandro Lagunas-Rangel
Biogerontology.2022; 23(1): 1. CrossRef - Protective effects of AdipoRon on the liver of Huoyan goose fed a high-fat diet
Zhongzan Cao, Ben Ma, Chengyu Cui, Jiahui Zhao, Sidi Liu, Yunqiao Qiu, Yan Zheng, Ming Gao, Xinhong Luan
Poultry Science.2022; 101(4): 101708. CrossRef - AdipoRon exerts opposing effects on insulin sensitivity via fibroblast growth factor 21–mediated time-dependent mechanisms
Yongliang Wang, Huan Liu, Ruixin Zhang, Yuyao Xiang, Junfeng Lu, Bo Xia, Liang Peng, Jiangwei Wu
Journal of Biological Chemistry.2022; 298(3): 101641. CrossRef - Compendious Review on Adipokines of Corpulence
Feryal Hashim
Research Journal of Pharmacy and Technology.2022; : 4315. CrossRef - AdipoR agonist increases insulin sensitivity and exercise endurance in AdipoR-humanized mice
Masato Iwabu, Miki Okada-Iwabu, Hiroaki Tanabe, Nozomi Ohuchi, Keiko Miyata, Toshiko Kobori, Sara Odawara, Yuri Kadowaki, Shigeyuki Yokoyama, Toshimasa Yamauchi, Takashi Kadowaki
Communications Biology.2021;[Epub] CrossRef - ADIPOR1 regulates genes involved in milk fat metabolism in goat mammary epithelial cells
Wangsheng Zhao, Michael Adjei, Hongmei Wang, Yueling Yangliu, Jiangjiang Zhu, Huijuan Wu
Research in Veterinary Science.2021; 137: 194. CrossRef - Differentiation of THP-1 monocytes to macrophages increased mitochondrial DNA copy number but did not increase expression of mitochondrial respiratory proteins or mitochondrial transcription factor A
Mizuho Okamoto, Masanori Shimogishi, Akari Nakamura, Yusuke Suga, Kyosuke Sugawara, Michio Sato, Ryotaro Nishi, Akio Fujisawa, Yorihiro Yamamoto, Misato Kashiba
Archives of Biochemistry and Biophysics.2021; 710: 108988. CrossRef - Clinical features, treatment and rehabilitation of new coronavirus infection in patients with metabolic syndrome
Dmitry O. Ivanov, Yury P. Uspenskiy, Andrey M. Sarana, Yulia A. Fominykh, Iana V. Sousova, Dmitry V. Zakharov
Pediatrician (St. Petersburg).2021; 12(5): 5. CrossRef - AdipoRon promotes diabetic fracture repair through endochondral ossification-based bone repair by enhancing survival and differentiation of chondrocytes
Zhongyi Wang, Jinxin Tang, Ying Li, Yu Wang, Yanyang Guo, Qisheng Tu, Jake Chen, Chen Wang
Experimental Cell Research.2020; 387(2): 111757. CrossRef - Discovery of AdipoRon analogues as novel AMPK activators without inhibiting mitochondrial complex I
Geng Sun, Yanping You, Haobin Li, Yalong Cheng, Ming Qian, Xinyu Zhou, Haoliang Yuan, Qing-Long Xu, Liang Dai, Pengfei Wang, Keguang Cheng, Xiaoan Wen, Caiping Chen
European Journal of Medicinal Chemistry.2020; 200: 112466. CrossRef - Insights Into the Controversial Aspects of Adiponectin in
Cardiometabolic Disorders
Emilio Antonio Francischetti, Rômulo Sperduto Dezonne, Cláudia Maria Pereira, Cyro José de Moraes Martins, Bruno Miguel Jorge Celoria, Patrícia Aguiar Cardoso de Oliveira, Virgínia Genelhu de Abreu
Hormone and Metabolic Research.2020; 52(10): 695. CrossRef - Adiponectin and Its Mimics on Skeletal Muscle: Insulin Sensitizers, Fat Burners, Exercise Mimickers, Muscling Pills … or Everything Together?
Michel Abou-Samra, Camille M. Selvais, Nicolas Dubuisson, Sonia M. Brichard
International Journal of Molecular Sciences.2020; 21(7): 2620. CrossRef - AdipoRon, a new therapeutic prospect for Duchenne muscular dystrophy
Michel Abou‐Samra, Camille M. Selvais, Raphael Boursereau, Sophie Lecompte, Laurence Noel, Sonia M. Brichard
Journal of Cachexia, Sarcopenia and Muscle.2020; 11(2): 518. CrossRef - Targeting perivascular and epicardial adipose tissue inflammation: therapeutic opportunities for cardiovascular disease
Rim Rafeh, Anissa Viveiros, Gavin Y. Oudit, Ahmed F. El-Yazbi
Clinical Science.2020; 134(7): 827. CrossRef - Therapeutic effects of AdipoRon on liver inflammation and fibrosis induced by CCl4 in mice
Min Sha, Yaru Gao, Can Deng, Yuemeng Wan, Yuan Zhuang, Xiaochuan Hu, Ying Wang
International Immunopharmacology.2020; 79: 106157. CrossRef - AdipoRon: A Novel Insulin Sensitizer in Various Complications and the Underlying Mechanisms: A Review
Ishfaq Ahmad Bhat, Shaheen Wasil Kabeer, Mohammad Irshad Reza, Reyaz Hassan Mir, Muhammad Ovais Dar
Current Molecular Pharmacology.2020; 13(2): 94. CrossRef - Case Report: Concurrent Resistance and Aerobic Training Regulate Adiponectin Expression and Disease Severity in Multiple Sclerosis: A Case Study
Elisa Grazioli, Ersilia Nigro, Claudia Cerulli, Giovanna Borriello, Annamaria Mancini, Eliana Tranchita, Rita Polito, Attilio Parisi, Pasqualina Buono, Aurora Daniele
Frontiers in Neuroscience.2020;[Epub] CrossRef - Mechanisms of Adiponectin Action: Implication of Adiponectin Receptor Agonism in Diabetic Kidney Disease
Yaeni Kim, Cheol Whee Park
International Journal of Molecular Sciences.2019; 20(7): 1782. CrossRef - Drug development research for novel adiponectin receptor-targeted antidiabetic drugs contributing to healthy longevity
Miki Okada-Iwabu, Masato Iwabu, Toshimasa Yamauchi, Takashi Kadowaki
Diabetology International.2019; 10(4): 237. CrossRef - Potential Role of Adiponectin Receptor Agonist, AdipoRon in Cardiometabolic Disease
Eunhee Cho, Sewon Lee
Exercise Science.2019; 28(2): 102. CrossRef - Adiponectin for the treatment of diabetic nephropathy
Jun Young Lee, Jae Won Yang, Byoung Geun Han, Seung Ok Choi, Jae Seok Kim
The Korean Journal of Internal Medicine.2019; 34(3): 480. CrossRef - Adiponectin receptor agonist AdipoRon relieves endotoxin-induced acute hepatitis in mice
Wen-Ze Xiao, Li Zhang
Chinese Medical Journal.2019; 132(20): 2438. CrossRef - Adiponectin/AdipoR Research and Its Implications for Lifestyle-Related Diseases
Masato Iwabu, Miki Okada-Iwabu, Toshimasa Yamauchi, Takashi Kadowaki
Frontiers in Cardiovascular Medicine.2019;[Epub] CrossRef - Examining the Potential of Developing and Implementing Use of Adiponectin-Targeted Therapeutics for Metabolic and Cardiovascular Diseases
Ying Liu, Vivian Vu, Gary Sweeney
Frontiers in Endocrinology.2019;[Epub] CrossRef - The role of immune cells in the development of adipose tissue dysfunction in cardiovascular diseases
E. G. Uchasova, O. V. Gruzdeva, Yu. A. Dyleva, E. V. Belik, O. L. Barbarash
Russian Journal of Cardiology.2019; (4): 92. CrossRef - Adiponectin and Inflammation in Health and Disease: An Update
Alice G. Geagea, Samir Mallat, Charbel F. Matar, Raymond Zerbe, Estelle Filfili, Maria Francis, Hanine Haidar, Abdo Jurjus
Open Medicine Journal.2018; 5(1): 20. CrossRef - Structure and function analysis of adiponectin receptors toward development of novel antidiabetic agents promoting healthy longevity
Miki Okada-Iwabu, Masato Iwabu, Toshimasa Yamauchi, Takashi Kadowaki
Endocrine Journal.2018; 65(10): 971. CrossRef - Adiponectin induced AMP-activated protein kinase impairment mediates insulin resistance in Bama mini-pig fed high-fat and high-sucrose diet
Miaomiao Niu, Lei Xiang, Yaqian Liu, Yuqiong Zhao, Jifang Yuan, Xin Dai, Hua Chen
Asian-Australasian Journal of Animal Sciences.2017; 30(8): 1190. CrossRef - The role of adiponectin receptors in the regulation of synaptic transmission in the hippocampus
Filippo Weisz, Sonia Piccinin, Dalila Mango, Richard Teke Ngomba, Nicola B. Mercuri, Ferdinando Nicoletti, Robert Nisticò
Synapse.2017;[Epub] CrossRef - Unravelling the adiponectin paradox: novel roles of adiponectin in the regulation of cardiovascular disease
Lavinia Woodward, Ioannis Akoumianakis, Charalambos Antoniades
British Journal of Pharmacology.2017; 174(22): 4007. CrossRef - Annual banned‐substance review: analytical approaches in human sports drug testing
Mario Thevis, Tiia Kuuranne, Hans Geyer, Wilhelm Schänzer
Drug Testing and Analysis.2017; 9(1): 6. CrossRef - Discovery of Novel Insulin Sensitizers: Promising Approaches and Targets
Yadan Chen, Haiming Ma, Dasheng Zhu, Guowei Zhao, Lili Wang, Xiujuan Fu, Wei Chen
PPAR Research.2017; 2017: 1. CrossRef - Adiponectin and Its Receptors in Diabetic Kidney Disease: Molecular Mechanisms and Clinical Potential
Dongqing Zha, Xiaoyan Wu, Ping Gao
Endocrinology.2017; 158(7): 2022. CrossRef - Role of pro- and anti-inflammatory phenomena in the physiopathology of type 2 diabetes and obesity
Luciano Pirola, José Candido Ferraz
World Journal of Biological Chemistry.2017; 8(2): 120. CrossRef - Perivascular adipose tissue as a regulator of vascular disease pathogenesis: identifying novel therapeutic targets
Ioannis Akoumianakis, Akansha Tarun, Charalambos Antoniades
British Journal of Pharmacology.2017; 174(20): 3411. CrossRef - Insight into the Dissociation of Behavior from Histology in Synucleinopathies and in Related Neurodegenerative Diseases
Kazunari Sekiyama, Yoshiki Takamatsu, Wakako Koike, Masaaki Waragai, Takato Takenouchi, Shuei Sugama, Makoto Hashimoto
Journal of Alzheimer's Disease.2016; 52(3): 831. CrossRef - Castration induced browning in subcutaneous white adipose tissue in male mice
Osamu Hashimoto, Tatsuya Noda, Atsushi Morita, Masahiro Morita, Hirofumi Ohtsuki, Makoto Sugiyama, Masayuki Funaba
Biochemical and Biophysical Research Communications.2016; 478(4): 1746. CrossRef - Aldosterone Production and Signaling Dysregulation in Obesity
Andrea Vecchiola, Carlos F. Lagos, Cristian A. Carvajal, Rene Baudrand, Carlos E. Fardella
Current Hypertension Reports.2016;[Epub] CrossRef
- Identification of a novel adiponectin receptor and opioid receptor dual acting agonist as a potential treatment for diabetic neuropathy

 KDA
KDA
 First
First Prev
Prev





